By Richard Queen
“Our health care system is designed to address medical fires versus fire prevention.”
Quoted in a study titled “Most Adults Don’t Receive Preventive Care,” Dave Chase, co-founder of Health Rosetta, speaks of the need for reform in traditional fee-for-service U.S. health care. While industries like manufacturing have long understood the need for preventative maintenance, realizing proactive equipment maintenance is far cheaper than loss of production and more expensive logistics, most of health care continues to operate by waiting until our bodies are broken.
“We spend far more to get far less,” says Chase.
According to a brief titled “A Generation of Healthcare in the United States: Has Value Improved in the Last 25 Years?,” U.S. spending on health care has held pace with peer countries while lagging behind in improvements to life expectancy and disease burden.So, while it may be more accurate to say the U.S. has spent the same to get less, many would agree with Chase’s sentiment that a more proactive care model is needed that prioritizes preventive and chronic care.
Chronic diseases such as heart failure, diabetes, asthma and others have been a large focus in recent years due to continued growth in the cost of treatment. A diabetic patient, for example, has medical expenditures approximately 2.3 times higher than a patient with the absence of diabetes, according to “The Cost of Diabetes Care—And How to Help Patients Lower It,” an article that appeared in Managed Healthcare Executive. In 2015, the Centers for Medicare and Medicaid Services implemented the Chronic Care Management (CCM) program, focusing on preventative care for those with two or more chronic disease conditions. While the CCM program has made great strides, waiting until one already has multiple diagnosed illnesses to begin preventative maintenance has shown limited success.
“Using prevention strategies from the very beginning is key,” says Dr. Joshua Joseph, an endocrinologist and assistant professor at The Ohio State University Wexner Medical Center who is researching ways to prevent diabetes.
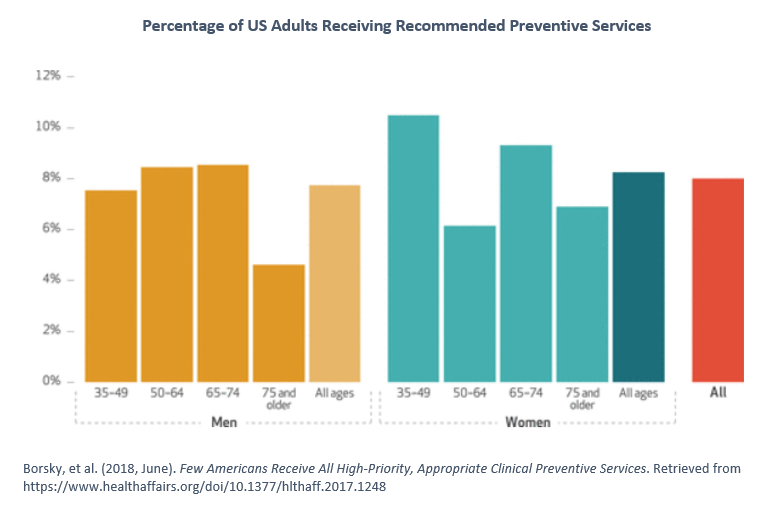
Unfortunately, a recent study revealed that only 8 percent of adults ages 35 and older receive all the highly recommended preventative services needed. With more than 50 preventative metrics published—each with different relevancies for age, gender, medical history and social determinants—it has become apparent that technology is needed to assist in ensuring the right preventative care is prioritized.
“The health care system needs to work together to encourage innovation on how care is delivered, how we can use new technology and how we can tailor improvements to meet the needs of local communities,” says Amanda Borsky, an employee of the Agency for Healthcare Research and Quality who led this recent study.
This statement may sound dated, given that electronic medical records (EMR) have been around for years, finding their beginning as the solution to a similarly stated problem—the need for innovation in medicine. However, EMRs now find themselves as the accounting systems of health care, tracking historical and transactional health encounters rather than providing insight into needed care. To utilize Hume’s law, EMR systems provide what is, when what is needed is the ought of proactive patient care.
The solution lies in being able to offer real-time patient screening for personalized medicine with actionable insights at the point of service. The benefit of EMRs is that they provide most of the patient data needed for such a task. It can be argued that the largest untapped asset of any health care organization is the data contained within their own EMR. The question is whether they are utilizing it effectively, turning data into information with which to drive decisions. Visualization platforms such as Microsoft Power BI and Tableau make this a much less intimidating and much more affordable endeavor. For most health systems, the issue is not knowing where to start. Analysis paralysis leaves them hesitant to take a step and instead they turn back toward their EMR accounting system for population health and preventative care. This assures one will pay far more and receive far less.
With minimal technical resources, patient data can begin to be extracted from a provider’s EMR and used to identify care opportunities. By utilizing elements such as patient demographics, lab results, transactional charge code history and vital signs, most preventative care metrics can be mapped and identified proactively. For instance, by utilizing a diagnosis code history, all diabetic patients can be identified. By combining that with patient lab results, all diabetic patients who did not receive a Hemoglobin A1C test in the last year can be identified. This happens to be an extremely relevant metric for diabetic patients. This process can be repeated for the approximately 30 measures that most value-based payer contracts are built upon, ensuring quality patient care. Visualizing these into actionable dashboards can offer real-time screening and, taken a step further by integrating into the patient schedule, allow care gap closure to happen at the point of service.
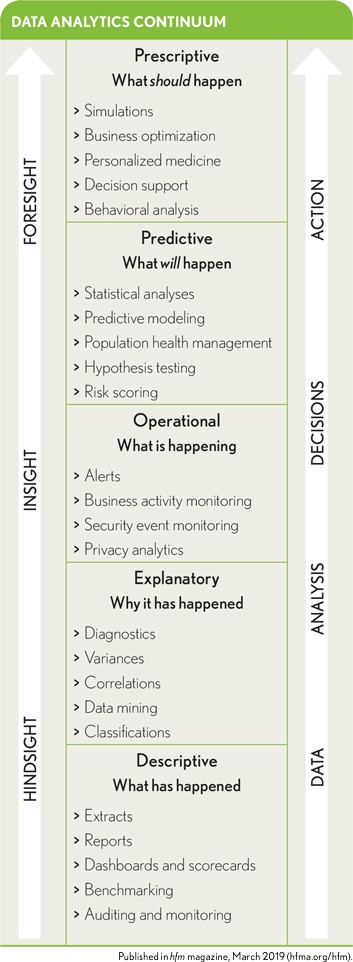
While this may be a simplistic example, it would not take many metrics built in this manner to begin making an immediate impact on patient care. Many health systems have entire quality departments dedicated to monitoring these patient metrics and working manually with payers to close care gaps. Much of the time, they are working with payer data that is six to nine months past the patient’s date of service. By utilizing EMR data with real-time screening built into the patient schedule the positive downstream impacts can be exponential.
First and foremost, first-class preventative patient care can be offered. With metrics built in the proper manner, a predictive quality can be achieved, and a health system can proactively engage patients at high risk. Quality scores will increase due to increased preventative medicine being offered and care gaps being closed. Population health and quality departments will work much more efficiently with tools in place to easily identify target patients, offering personalized medicine rather than a shotgun approach to chronic disease management. For the system concerned about the unpredictability of revenue, most preventative care services are covered at 100 percent by the payer, knowing that when preventative care is offered, patients are better managed and emergency room utilization and hospitalizations decrease. With these goals being aligned in any value-based provider contract, payer savings are easily achieved and gainsharing can take place—the definition of success in any ACO or risk-based arrangement.
Known as the domino effect, a simple domino can knock down another domino 1.5 times its size. The key is to knock down the first domino. Instead of being paralyzed by incomplete information, a health system can start with EMR data and knowledge of payer contracts, combining them to affect change. Just like the dominos, adding automation around preventative medicine can have exponential impacts in any care environment. By raising preventative medicine coverage from the 8 percent referenced above, chronic disease can be better managed and health care costs could actually begin to decrease rather than just slowing the rate of growth. It is possible to pay far less and receive far more.
About the Author

Richard Queen is vice president of data science for IntelliGap, a software solution focused on closing gaps in preventative patient health care by utilizing real-time, personalized patient screening and actionable insights from existing medical records.








